Research study suggests that SARS-CoV-2– the infection that triggers COVID– can straight assault the epithelial cells that line the GI system, going into by means of the molecular entrance of angiotensin‐converting enzyme 2 (ACE2). These cells reveal high levels of ACE2, as do the cells lining the lungs, the main website of infection.
However the gut is not simply a passive target for the infection. Proof recommends it is likewise a gamer in identifying the intensity of COVID-19 A burst of research study over the previous years has actually revealed that the small citizens of the gastrointestinal system– the gut microbiota– play an essential function in securing the body from pathogens and in controling immune actions to infections, which appears to be the case for COVID.
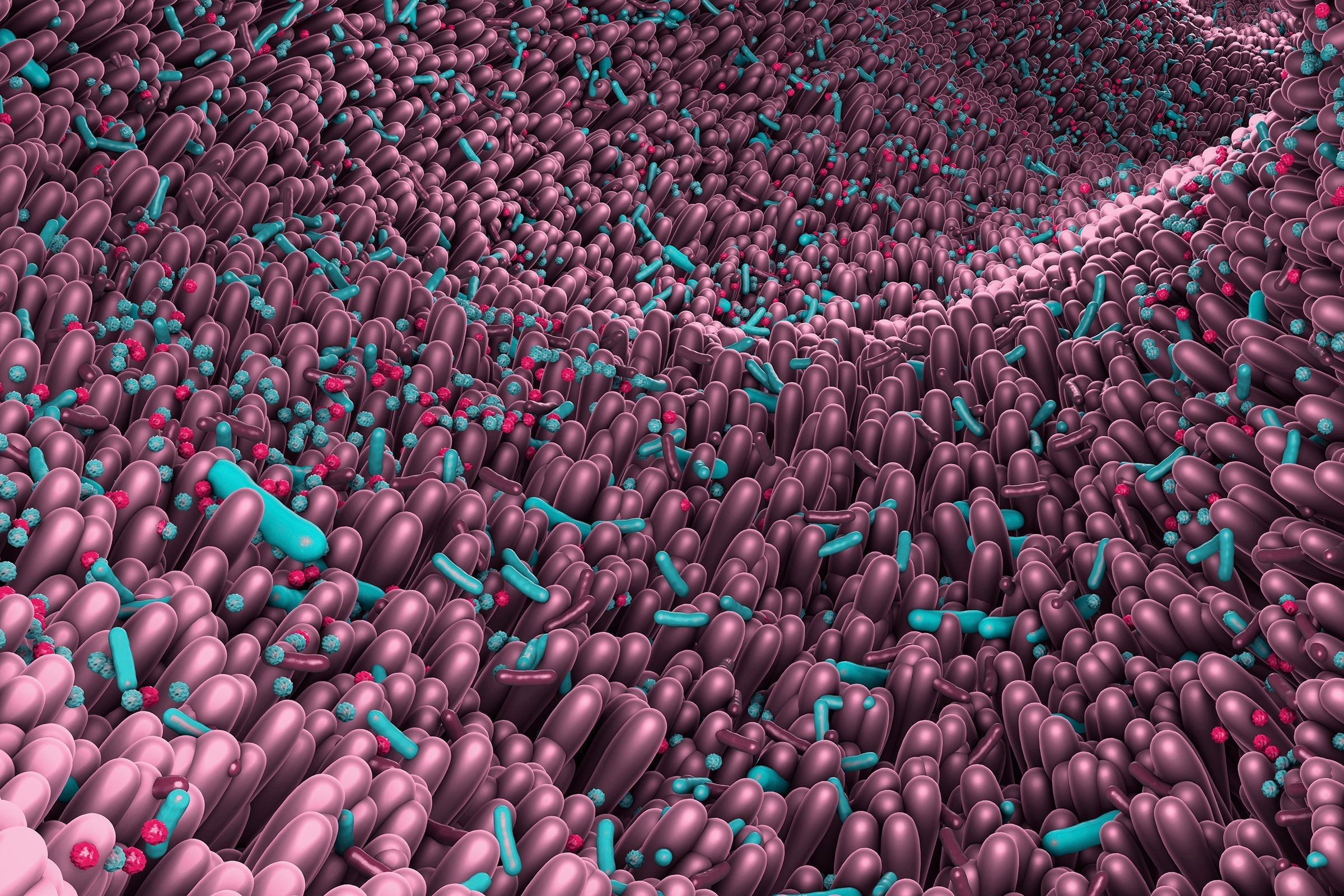
Trillions of germs, fungis, infections and other single-celled organisms live in the intestinal system in a vibrant, commensal community. And each people harbors our own special neighborhood. When our gut microbiota remain in a varied however healthy and well balanced state, they support the appropriate performance of our body immune system. When the balance is disturbed– a condition researchers call dysbiosis– our defenses are jeopardized, and we are more prone to infections.
The variety of the gut microbiota is understood to decrease with increasing age And likewise, there is an association in between transformed gut microbiota and persistent illness, such as weight problems, diabetes and heart disease– conditions that incline people to serious COVID-19 There isn’t yet evidence of a direct relationship in between COVID intensity and gut dysbiosis, however proof is installing.
In a 2021 research study of 100 clients hospitalized with COVID, Siew C. Ng and her associates at the Chinese University of Hong Kong discovered that, in general, the topics’ gut microbiome (as determined in stool samples) was substantially less varied than samples drawn from a prepandemic control group, no matter whether the clients had actually taken prescription antibiotics or other drugs. A variety of useful bacterial types lacked COVID clients, and the degree of microbiome disruption associated with illness seriousness and increased indications of swelling.
” Numerous gut microbes with recognized immunomodulatory function were diminished in clients with COVID-19,” Ng describes. Their exhaustion may be a consider the “cytokine storm,” the harmful, hyperinflammatory state that is often seen in COVID clients, states Ng, who is associate director of the Chinese University of Hong Kong’s Center for Gut Microbiota Research Study.
That circumstance is among numerous methods which our gut citizens might affect COVID seriousness. The exact systems are not yet understood, “however we can assume,” states Harry Sokol, who studies the relationship in between gut microorganisms and the body immune system at Saint-Antoine Healthcare facility in Paris. He recommends that “in the early stage of infection, there is a change of the gut microbiota resulting in a reduced production of microbiota-derived [substances] that are necessary to manage the infection.” Such modifications were observed in a 2021 research study led by Sokol in which macaques were contaminated with SARS-CoV-2.
In a later stage of COVID, Sokol recommends, the decrease in specific microorganisms may affect the stability of the gut. These microorganisms usually create compounds that assist keep the gut lining, consisting of short-chain fats such as butyric acid. Lower levels of essential germs may for that reason trigger a” dripping gut,” which, in turn, might trigger pro-inflammatory particles to seep out, increase cytokine storms that can trigger the substantial organ damage seen in extreme COVID cases.
Damage to the gut itself– and to other organs– might be the outcome of swelling, the viral attack itself or the disturbance of ACE2’s regular functions. In the gut, ACE2 plays lots of functions consisting of managing the ecology of the gut microbiota. Therefore, it is unclear if COVID triggers an unhealthy gut or if an unhealthy gut sets the phase for extreme COVID. “Most likely both hold true and connected,” Sokol states.
Gut microorganisms might affect COVID results through an exchange of chemical signals with cells in the lungs. This just recently found “gut-lung axis,” like a lot of biological axes, is a two-way affair: digestive microorganisms affect how the lungs react to infections, and lung swelling can likewise modify the gut microbiota. A evaluation research study by Brazilian researchers that was released previously this year discovered that research study revealed that chemical signals sent out by gut germs and gotten by cells in the lungs can assist safeguard mice from infection with an influenza infection, whereas offering mice prescription antibiotics that interrupt their gut microbiota compromises their immune reaction to influenza. If the exact same holds true for COVID in people, clinicians need to beware about utilizing prescription antibiotics in COVID clients– unless, obviously, they have secondary microbial infections.
As researchers discover more about the function of the gut in COVID, there might be other ramifications for treatment and avoidance. Keeping an eye on gut health might be one method to anticipate seriousness, and utilizing probiotics and enhanced diet plan to increase the microbiome may show to be an important technique. Ng keeps in mind that numerous randomized trials with a specifically created mix of probiotics are underway at her organization: these trials intend to decrease the threat of COVID in susceptible groups such as the senior and individuals with diabetes and to enhance reaction to COVID vaccines. Other scientists are likewise checking the possible advantages of utilizing probiotics and of transplanting fecal organisms to COVID clients with lacking gut populations.
There might even be lessons for the dreadful “long COVID.” In their 2021 research study, Ng and her coworkers discovered that gut dysbiosis continued numerous recuperated COVID clients when the infection was no longer noticeable which it might add to continuous illness. The research study followed some clients for 30 days after healing, and the authors think longer follow-up of this problem is necessitated. It might be a good idea, Ng states, for “retrieved clients to take in diet plans or integrate activities understood to be helpful for the gut microbiome: increasing fiber consumption, taking probiotics and working out.” It’s sound recommendations under any situation.
This short article belongs to an editorially independent Springer Nature collection that was produced with financial backing from Lonza
No comments:
Post a Comment